Abstract
Background:Von Willebrand disease (VWD) is a common congenital bleeding disorder, caused by defective or deficient von Willebrand factor (VWF), and characterized by mucosal bleeding. Among these, recurrent gastrointestinal (GI) bleeding may be serious and life-threatening,requiring hospitalization in 30%. Diagnosis and management remain challenging, and the prevalence and correlates of GI bleeding in VWD are not well understood.
Methods. We conducted a cross-sectional study using discharge data from the National Inpatient Sample (NIS) between January 1, 2009 and December 31, 2014 to identify factors associated with GI bleeding in VWD. NIS is the largest publicly available inpatient database in the U.S. developed by Healthcare Cost and Utilization Project (HCUP), containing a 20% stratified sample of U.S. hospital discharges. Discharges of individuals with and without VWD were evaluated by age, race, gender, primary and secondary diagnoses, length of stay, insurance, and discharge status. International Classification of Diseases, 9thedition, Clinical Modification (ICD9-CM) codes were used to classify de-identified discharge data by causes of GI bleeding, medications, blood products, and comorbidities. Discharge-level weights from the NIS database were used to produce estimates representative of all U.S. community hospitals. We compared GI bleeding prevalence between patients with and without VWD, and among those with VWD, the demographics (age, gender, race), length of stay, inpatient mortality, payor, medical comorbidities, and potential causes of and risk factors for GI bleeding. Categorical variables were compared by Rao-Scott chi-square test, and continuous variables by weighted simple linear regression. Independent factors associated with GI bleeding in VWD were determined by a weighted multivariable logistic regression model.
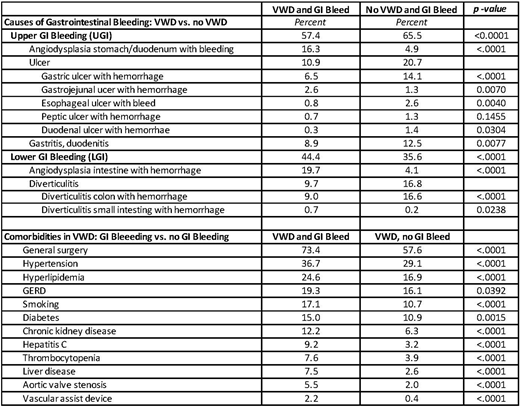
Results:Individuals with VWD and GI bleeding were younger than those without GI bleeding, 58.5 yr vs 45.2 yr, and were more likely male, 42.3% vs 25.9%, and Black, 12.3% vs 7.5%, each p<0.0001. Overall, the prevalence of upper GI bleeding (UGI) was greater than lower GI bleeding (LGI) in VWD, 57.4% vs 44.4%; but these rates were significantly higher in non-VWD, 65.5% vs 35.6%, each p<0.001. The most common cause of GI bleeding in VWD was angiodysplasia, 36.5% (LGI 19.7%, UGI 16.3%) which was significantly more common than in non-VWD, 9.5% (LGI, 4.1%, UGI, 4.9%), p<0.0001. By contrast, the next most common causes of GI bleeding in VWD were ulcer disease, 10.8%; diverticulitis, 9.7%; and gastritis/ duodenitis, 8.9%, each less common than in non-VWD, 20.7%, 16.7%, and 12.5%, p<0.01. The most common ulcer type was gastric ulcer, 6.5% vs 14.1%, respectively, p<0.0001.
Among VWD patients, those with GI bleeding were more likely than those without GI bleeding to receive aspirin, 3.3% vs 2.0% (p=0.030), platelet transfusion, 4.0% vs 2.1% (p=0.0012), and coagulation factor, 7.8% vs 4.6% (p=0.0003). Comorbidities were also more common in VWD with GI bleeding, including surgery, 73.4% vs 57.6%; hypertension, 36.7% vs 29.1%; hyperlipidemia, 24.6% vs 16.9%; GERD, 19.3% vs 16.1%; smoking, 17.1% vs 10.7%); diabetes, 15.0% vs 10.9%; chronic kidney disease, 12.2% vs 6.3%; hepatitis C, 9.2% vs 3.2%; thrombocytopenia, 7.6% vs 3.9%; liver disease, 7.5% vs 2.6%; aortic valve disease, 5.5% vs 2.0%; and vascular assist device, 2.2 vs 0.4%, each p<0.0001. Severity of illness, 1.5 vs 0.9, p<0.0001, and inpatient mortality, 2.4% vs 1.2%, p=0.011 were higher in VWD with GI bleeding than without GI bleeding.
In a multivariable model, variables significantly associated with GI bleeding in VWD were angiodysplasia, OR=104.06 [95% CI: 75.14, 144.11]; diverticulitis, OR=16.66 [11.85, 23.42]; hepatitis C, OR=2.17 [1.40, 3.36]; Black race, OR=1.80 [1.31, 2.47]; male gender, OR=1.61 [1.29, 1.99]; and smoking, OR=1.40 [1.04, 1.88].
Conclusion.The most significant correlates of GI bleeding in VWD are angiodysplasia, diverticulitis, hepatitis C, Black race, male gender, and smoking. Identification of VWD at high risk for GI bleeding with consideration for factor prophylaxis after the first GI bleed, may help reduce the morbidity of recurrent GI bleeding in VWD.
Ragni:Bioverativ: Consultancy, Research Funding; CSL Behring: Research Funding; MOGAM: Membership on an entity's Board of Directors or advisory committees; Shire: Research Funding; SPARK: Consultancy, Research Funding; Alnylam: Membership on an entity's Board of Directors or advisory committees, Research Funding; Biomarin: Membership on an entity's Board of Directors or advisory committees, Research Funding; Novo Nordisk: Research Funding; Sangamo: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal